A 42 year old male patient came with hiccups since three days
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
A 42-year-old male patient carpenter by occupation came to the casualty with the
CHIEF COMPLAINTS:-
Hiccups for three days,
Pain abdomen for two days,
Vomiting for two days.
HISTORY OF PRESENT ILLNESS:-
He was apparently asymptomatic two years back then he had developed yellow discoloration of the sclera for which he visited a nearby hospital and got treated conservatively (MEDICATION: UDILIV for how many days? INDICATION?) One year back, he again had Sclera, for which the patient took UDILIV and the discoloration decreased.
Ten days back, the Patient had an injury to the right-hand ring finger (laceration of size 1*1cm over the dorsum), due to an accidental hit while working in the carpenter shop. later the injury, the whole hand got swollen. There was mild tenderness all over the hand, and after that, he cannot flex his ring finger.
Five days back he got a fever associated with chills and rigor, and after consulting a hospital then he started medication (PIPTAZ INJ.) then the fever got subsided and he had no history of weight loss, no diurnal variation.
For three days, he is suffering from continuous hiccups and got relieved temporarily from drinking water and the hiccups continued as soon as he vomited water. For two days he is having Abdominal pain ( Right- upper Abdomen).
there are at least 15 to 20 vomitings in two days, Non-Bilious Non-projectile food and water as contents.
There is a complaint of decreased urinary output since yesterday and constipation for two days.
past history:-
diabetic ( type 2) for 5 years under medication (Metformin, Teneligliptin) and is under control.
medication (oral drugs)
not a known case of HTN, epilepsy, CAD, asthma, TB, leprosy
personal history:-
appetite - normal
diet - mixed
bowel and bladder - regular
sleep adequate - adequate
addictions - regular (alcohol 180ml since?)
no tobacco drug usage
FAMILY HISTORY:-
no significant family history
Allergic history:-
not allergic to any kind of drugs or food.
occupational history:-
he is a carpenter
GENERAL EXAMINATION:-
the patient is conscious co-operative and well oriented towards time place and person.
well built and well nourished
VITALS:-
temperature:-Afebrile
pulse rate:- 80 bpm
respiratory rate:-20 CPM
B.P:-120/90 mm Hg
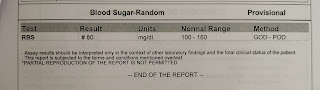
GRBS:- 115 mg%
B.M.I:-?
SPO2:- 99%
Pallor - No
Icterus - present
Cyanosis - No
Clubbing - No
Lymphadenopathy - No
Edema - No
SYSTEMIC EXAMINATION:-
FOR ABDOMEN:-
The shape of the abdomen - mild distension
Tenderness - present ( Right hypo chondrium, Epigastric region, Left hypo chondrium, Umbilical region)
No palpable masses
No free fluid
Liver -?
Spleen - Not palpable
Bowel sounds - Normal
RESPIRATORY SYSTEM:-
Bilateral air entry - Positive
Normal vesicular breath sounds are heard all over the chest
CARDIOVASCULAR SYSTEM:-
S1, S2 - Heard
No murmurs
CENTRAL NERVOUS SYSTEM:-
Speech - Normal
Cranial nerves - Normal
Motor system - Normal
Sensory system - Normal
No signs of meningeal irritation
INVESTIGATIONS:-
Dialysis done on
31/7;1/8;3/8
DIAGNOSIS:-
Leptospirosis with sepsis AKI, DM for 5 years
TREATMENT:-
Allow only water
INJ- NS, RL _ 100ml | HR
INJ PANTOP 40mg IV | BD
INJ XOFER 4 MG IV | TID
INJ THIAMINE 100mg IV 100ml NS IV | TID
INJ MONOCEF 1gm IV |BD
INJ DOXY 100mg IV| BD
TAB BACLOFEN 10mg PO | BD








































Comments
Post a Comment